EducationHealth and Safety Risks: Student Athletic Programs, On-Campus Camps, and Student Health Services
Q2 2024
Institutions of higher education take very seriously their charge to protect the health and well-being of students and visitors entrusted to their care. This includes protecting those individuals from their peers, the elements, injuries, illnesses, nefarious actors, random misfortune, and even themselves, as best they can.
College and university best practices related to due diligence, supervision, training, facility and equipment maintenance, and physical security can help reduce risk. Insurance-based risk transfer is an important backstop when even the best risk prevention strategies prove insufficient.
This report covers three areas of liability that higher education institutions may overlook regarding their responsibility for the health and well-being of those on their campuses: school athletic programs, camps for minors, and student health services.
“Coaching errors” cover a wide range of missteps or worse made by members of a coaching staff – not only paid or unpaid head coaches but also assistants and other volunteers.
One of the most common areas of coaching errors is failure to protect the health of participants and prevent physical harm against them.
In cases of accidents or athletic-related illnesses, in addition to the personal trauma suffered by the athlete and their family members, schools must also consider their own costs and risk exposure. Not all risks can be avoided in these situations, but it is imperative that educational institutions manage and plan for foreseeable risks in their athletic programs. If not, there is a very real possibility that the school will be found liable if incidents occur.
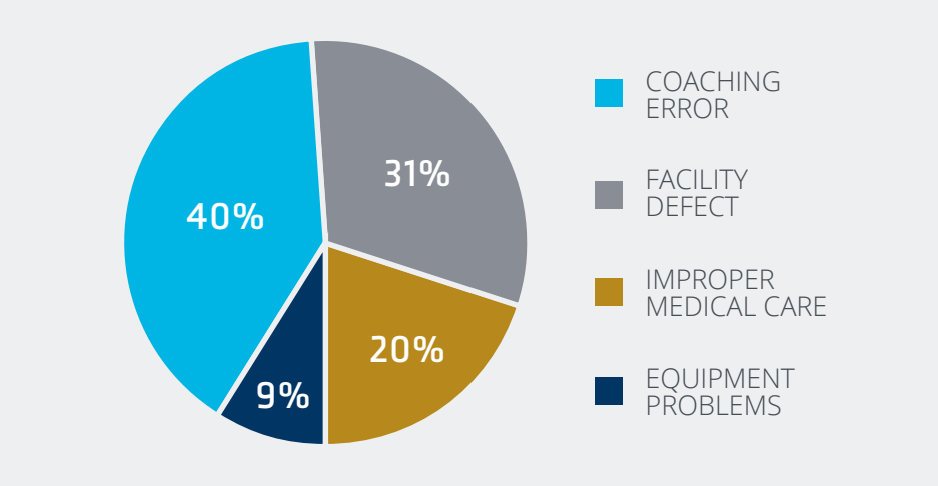
A United Educators analysis of liability claims data from intercollegiate and club athletics found that coaching errors were the most common cause of player injuries and were cited in 40% of claims with losses, with an average loss of more than $420,000.1
Student-athlete injuries occur relatively often even in low-contact sports. That’s largely due to heat-related illnesses, one of the most prevalent areas of healthrelated coaching errors. These conditions are brought on when the body’s natural cooling system has difficulty keeping up with physical exertion in a hot and often humid sporting environment, resulting in a rapid rise in body temperatures.
Although heat-related illnesses are preventable, they’re still a leading cause of death and disability for U.S. student-athletes.
The spectrum of heat-related illnesses is wide, ranging from mild conditions like heat rash and sunburn, to more serious issues such as cramping, heat exhaustion, and heat stroke. These situations can be effectively prevented with proactive programs that include:
What may first appear as fatigue or mild cramps, can quickly progress to life-threatening heat stroke. The initial symptoms of various types of heat illness are similar, including thirst, confusion, and headaches. Too often, staff members don’t always recognize these signs that the athlete is in distress.
Further, training seasons should be phased in to allow athletes to gradually adjust to heat over seven to 14 days, with gradual progression of duration and intensity of physical activity, exposure to heat, and use of equipment.
Hosting summer youth camps focused on academics or athletics is an excellent opportunity to introduce middle and high school students to the institution and develop longer-term ties. It’s an equally valuable way for these students to advance their skills as they utilize resources and learn from instructors they wouldn’t otherwise have access to.
While on campus, however, these students are vulnerable to unscrupulous instructors and others who might take advantage of a minor’s naivety or immaturity, leading to sexual abuse or other molestation incidents. These can inflict lifelong pain on a vulnerable individual and significantly damage the institution’s reputation.
Preventing incidents of this sort requires creating a safe environment for youth on campus. This begins with laying out detailed behavior guidelines for the faculty, staff, and volunteers who administer the program and all others on site. It also calls for clear instructions for the visiting students on inappropriate behavior by them and the staff, and instructions for safely reporting incidents.
Establishing camp-specific procedures to ensure a safe adventure for the visiting students involves fully documenting all camp activities and identifying areas of risk during all phases, including transportation, lodging, outings, and more. The plans should be prepared and reviewed by a committee comprised of a top administrator, chief financial officer, risk manager, human resources representative, legal counsel, and others.
These committee members should also be familiar with the organization’s liability coverage and exposures.
These plans should encompass best practices on areas including:
Most higher education institutions recognize that college-aged students are especially vulnerable regarding physical and mental well-being.
In response, student health coverage has paid close attention to mental health as students are more independent, which can impact medications being utilized. Institutions are increasingly facing limited resources on campus, fewer access points, and counselors and, therefore, reaching out with information on substance abuse, sexual health, contraception, mental health, and more.
Resources are limited within student health services, and the biggest preparation is needed with international students, as communication pre-enrollment and once on campus becomes paramount.
Supporting colleges and their student health services can be managed and leveraged in a few key ways:
In addition to the more common institutional risks in secondary education, such as cyber threats and mass attacks, this report includes important reminders regarding risks related to sports and recreation programs, visiting minors, and student health service programs.
In many ways, a college or university is a microcosm of the “real world,” with many of the same inherent risks and organizational liabilities. Colleges and universities are not necessarily ivory towers isolated from society. Their leaders are well-advised to consider all the risks they have in common with other “outside” organizations and adopt many of the same risk management and transfer strategies.
IMA maintains a team of experienced professionals dedicated to assisting institutions in coverage analysis, procedure review, training program review, and more.
Derek Karr
National Education Practice Director
Brenda Rice
Risk Control Advisor
David Bottoms
President, The Bottoms Group
Angela Thompson
Sr. Marketing Specialist, Market Intelligence & Insights
Brian Leugs
Writer
Soraya Marashi
Marketing Coordinator, Copy Editor