COVID-19
Telemedicine
Answers to a few of the most-discussed Telemedicine questions during COVID-19.
Coronavirus has had an impact on the ability of businesses to perform. It is prudent for businesses to review the information that may have lasting results on their relationships impacted by this pandemic.
Best practices for getting the most out of Telemedicine during Covid-19
As the number of COVID-19 cases surges across the country, patients, health care workers, and employers are struggling to ensure that people are receiving adequate care in a safe environment. Telemedicine allows health care professionals to evaluate, diagnose and treat patients at a safe distance, provide guidance to those who may be able to manage their symptoms at home, and help those who need elevated care access it quickly and efficiently.
While many companies have previously implemented telemedicine, the current need and demand is unprecedented. Here are a few best practices for employees and employers to get the most out of a telemedicine provider:
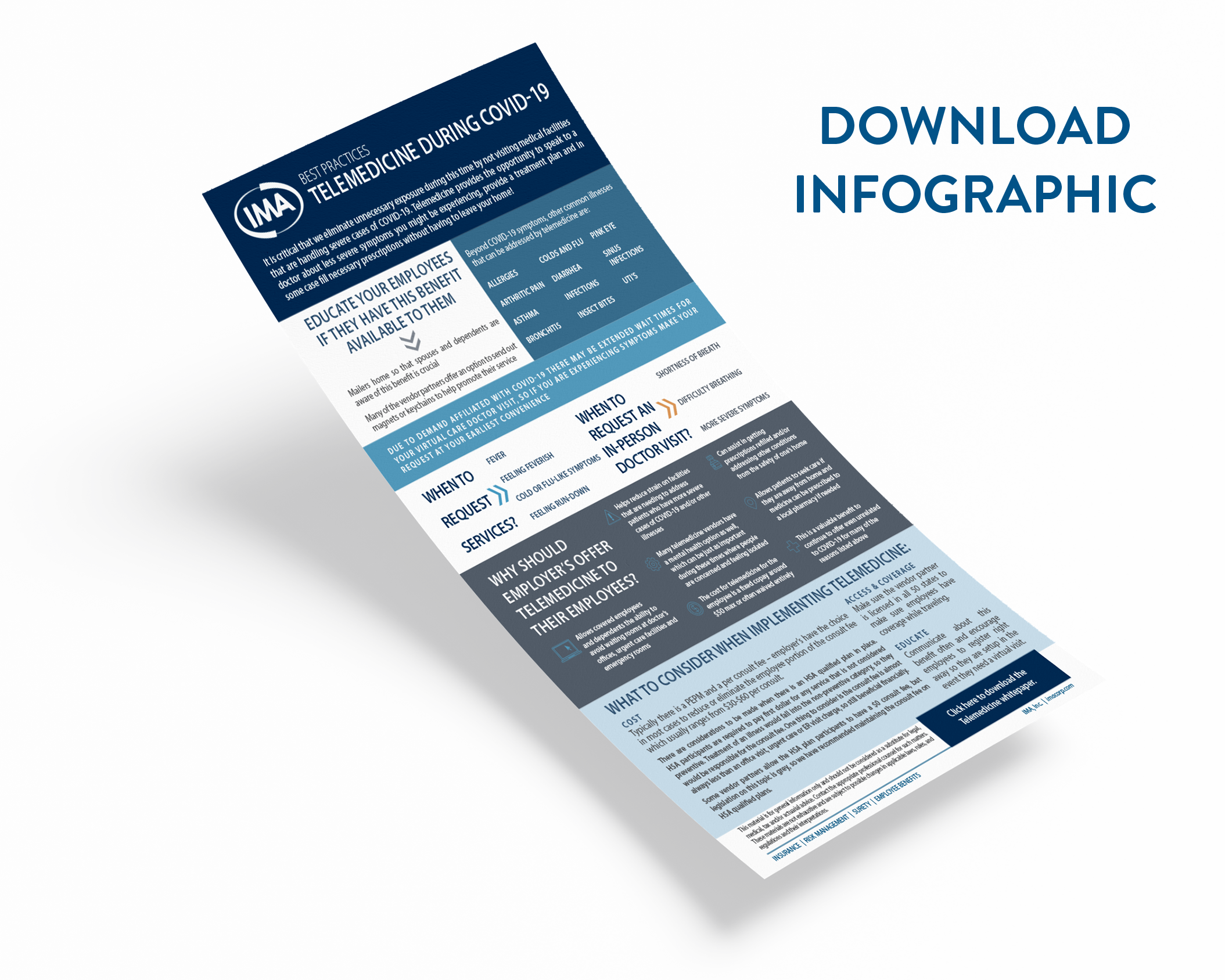
When should someone call request services?
All patients should be aware that due to high demand, there may be extended wait times for a virtual care doctor visit. If someone is experiencing any of the following symptoms, they should call at their earliest convenience:
Fever
Feeling feverish
Have cold or flu-like symptoms
Feel run-down
When should someone request an in-person doctor visit?
A telemedicine health provider will be able to help evaluate symptoms and recommend the next steps. The following may indicate a reason that the patient may request an in-person doctor visit for further evaluation, or the virtual care doctor may recommend it.
Shortness of breath
Difficulty breathing
More severe symptoms
What costs are typically associated with telemedicine for both employers and employees:
Most telemedicine plans will have a Per Employee Per Month (PEPM) cost and a per consult fee. Employers have the choice in most cases to reduce or eliminate the employee portion of the consult fee, which usually ranges from $30-$60 per consult.
If there is an HSA qualified plan in place, there are certain considerations; however, new legislation has been passed in the wake of COVID-19 that has changed HSA compliance in the treatment of COVID-19.
Typically, HSA participants are required to pay first dollar for any service that is not considered preventive. Treatment of illness would fall into the non-preventive category, leaving employees responsible for the consult fee. Some vendor partners allow the HSA plan participants to have a $0 consult fee, but legislation on this topic is grey.
One thing to consider is that the consult fee is almost always less than an office visit, urgent care or ER visit charge, so it may still be financially advantageous to use their telemedicine provider as the first line of defense.
However, for COVID-19 treatment and testing, IRS Notice 2020-15, high deductible health plans may cover COVID-19 testing and all subsequent treatment with low or no cost-sharing, without compromising the ability to contribute to a health savings account (HSA).
Why should employers offer telemedicine to their employees?
Telemedicine can work on the frontlines, reducing strain on facilities that are already experiencing an influx of patients with more severe cases of COVID-19 and/or other illnesses and injuries.
By using telemedicine services, employees and their covered family members can avoid sitting in waiting rooms at doctor’s offices, urgent care facilities and emergency rooms, keeping them and others safe.
For those who have regular prescriptions, telemedicine can allow patients to refill their prescriptions from home. If patients are traveling and have found themselves caught in a “shelter-in-place” order, not near their home, telemedicine can allow them to have their prescriptions filled by a local pharmacy.
Many telemedicine vendors have a mental health option as well, which can be just as important during these times where people are concerned and feeling isolated
Many employers should consider continuing to offer telemedicine coverage for many of these reasons, even after the COVID-19.
What to consider when choosing a telemedicine provider?
Access and Coverage: Make sure the vendor partner is licensed in all 50 states to make sure employees have coverage while traveling
Educate: Communicate about this benefit often and encourage employees to register right away, so they are set up in the event they need a virtual visit. Help your employees understand the advantages of the service and encourage them to use it for the appropriate situations.
IMA is a Resource
To learn more about how to get started offering telemedicine or to discuss in greater detail, please contact your local IMA Account Executive.